This is evident from a new study published in the journal Frontiers in endocrinologyresearchers have discovered that a commonly measured enzyme in routine blood tests, alkaline phosphatase (ALP), could serve as a marker for osteoporosis.
The study showed that higher ALP levels were consistently associated with a greater likelihood of osteoporosis, with stronger associations in metabolically younger females.
The great need for accessible biomarkers
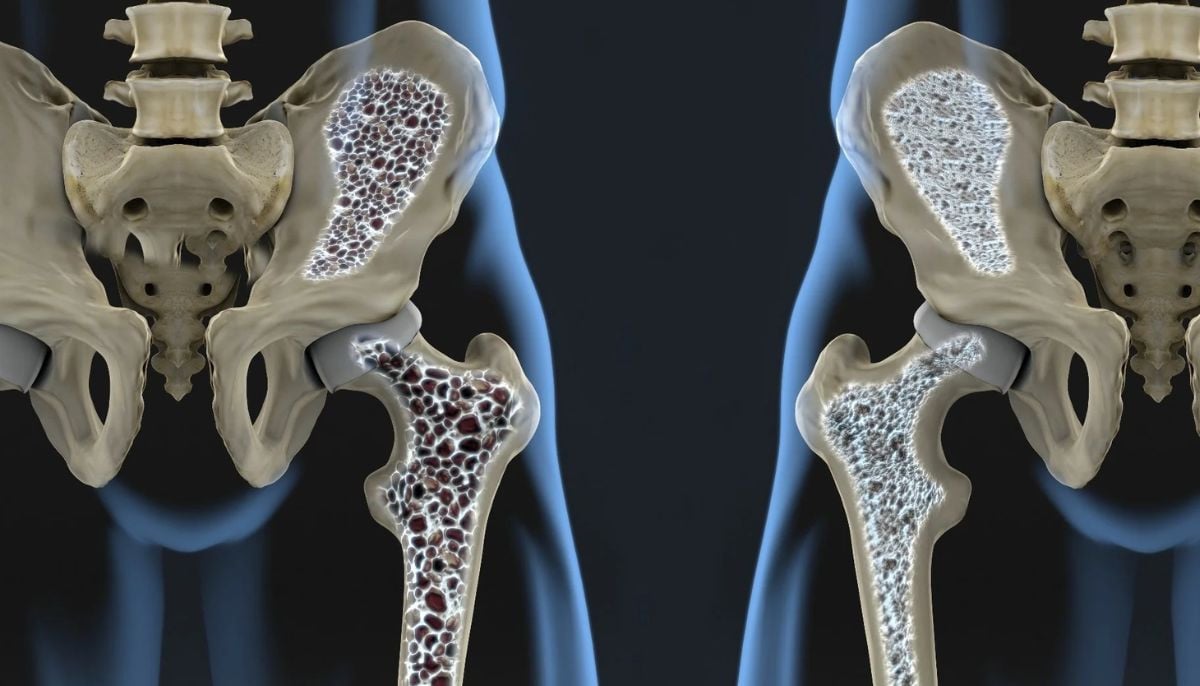
Osteoporosis is characterized by a reduction in bone mass and structural deterioration, leading to an increased risk of fractures and significant consequences for health and quality of life.
It has been observed that as fractures increase sharply with age, especially after 75 years, there is growing interest in identifying accessible biomarkers that can detect bone loss earlier.
ALP, produced mainly by bone-forming osteoblasts and hepatocytes, plays a crucial role in bone mineralization by breaking down pyrophosphate.
ALP is cheap and available at routine health checks, and researchers have explored its potential as a biomarker for bone health.
Researchers specifically analyzed whether total ALP can indicate osteoporosis risk in a large, systematically assessed population.
Eligible participants were adults aged 20 years or older who completed ALP testing and dual-energy X-ray absorptiometry (DXA) scans of the hip and spine.
It has been observed that hospital procedures were used to collect anthropometric measurements, blood pressure, ultrasound findings and biochemical markers including glucose, lipids, uric acid and liver enzymes.
While among the 12,835 participants, 9.5% were diagnosed with osteoporosis, and almost all individuals had ALP levels within the clinical reference range. Participants with osteoporosis had elevated ALP levels.
Subgroup differences and metabolic influences
Subgroup analysis showed stronger statistical associations rather than higher risk in women, younger individuals and those with normal liver enzymes and healthier metabolic profiles.
When liver enzymes were elevated, or when glucose or lipid profiles were abnormal, this association disappeared, while it was suggested that metabolic and hepatic factors may confound the association between bone status and ALP.
This study analyzed that higher serum total ALP is closely associated with a higher risk of osteoporosis.
The association was strongest in younger women and metabolically healthy individuals, because ALP more accurately reflects ALP when liver function and metabolic status are normal.
Nevertheless, the strengths of the study include the standardized clinical data and detailed subgroup analysis.
The study does not include information on physical activity, thyroid status, medication use and diet, which limits the findings.
Furthermore, it may serve as a preliminary limit for further assessments of bone health, although longitudinal cohort studies are needed to substantiate its causal and predictive estimation.