A decades of old pill remains useful for patients with a heart attack, even with modern treatments that can prevent permanent damage to the heart muscle, have shown two major studies.
It is still unclear whether all patients, or just a few, benefit from so-called beta-blocker drugs, which are usually prescribed to everyone after a heart attack.
Two sharp contradictory reports were presented on Saturday during a large cardiology meeting in Madrid and published in the New England Journal of Medicine.
“It is not unusual for testing to produce different results,” said Dr. Borja Ibanez van Centro Nacional The Investigaciones Cardiovasculares Carlos III in Madrid, who led one of the tests.
“It is somewhat unusual to see two tests with apparently different findings presented on the same day.”
The most important thing, Ibanez said, is the finding that both teams agree, namely that beta -blockers reduce the combined risk of another heart attack, heart failure or death in patients without heart failure, but with a mildly reduced heart function.
The question is whether the pills are favorable or useless for people with normally functioning hearts, who are good after a first heart attack about 80% of patients.
Beta-blocker-fabrikanten zijn onder andere Mylan, Novartis, Opens New Tab, Pfizer, Opens New Tab, Abbott, Teva Pharmaceutical Industries, Opens New Tab, Amneal Pharmaceuticals, Opens Nieuwe Tab, Sun Pharmaceutical Industries, Opens New Tab, Lupin, Lupine, ANI Pharmaceutics, Opens Nieuwe Tab en Eagle Pharmuticals, Open new tab.
The drugs work by inhibiting the hormones epinephrine and norepinephrine, reducing heart rate and blood pressure, reducing the workload on the heart and reducing the oxygen demand.
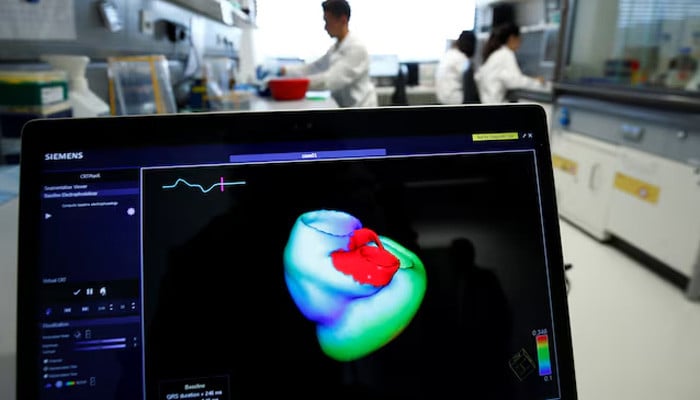
Both new tests concerned survivors of a heart attack whose hearts still contract normally, meaning that the left ventricle pumped at least 40% of its blood with each beat. Both studies followed patients for about 3.5 years.
Of the 5,574 volunteers in the Betami -Danblock study from Norway and Denmark, the medicines showed a clear advantage. Patients who were randomly allocated to receive beta -blockers had a 15% lower risk of death or a large adverse cardiovascular event, in particular a repeated heart attack compared to patients who do not use these pills, researchers found.
But among 8,438 participants in the reboot study in Italy and Spain, beta-blockers had no effect on the incidence of death for whatever cause, a repeated heart attack or hospitalization for heart failure, according to a separate report.
Some of the differences may be due to the fact that patients did not all receive the same beta -blockers, and the Scandinavian patients were perhaps more susceptible to side effects because they were slightly older than patients in Spain and Italy and more of them had mild heart dysfunction, Dr. Then Atar from the University of Oslo, which led one of the substances.
Among female participants in reboot, those who take beta-blockers, especially who, with a good heart function that had higher doses, had adverse results than women who do not use the drugs, researchers reported in the European Heart Journal.
In the re -start -up, researchers saw a lower speed of new heart attacks, heart failure or death with beta -blocker use by patients with a mildly reduced heart function, as indicated by a left ventricular “ejective fraction” between 40% and 49%.
The effect in this subgroup was confirmed in an analysis of data combined from reboot, betami -danblock and a Japanese test, published in the Lancet according to a report.
The message for cardiologists, Ibanez said, is: “We can now say that beta -blockers are favorable” in patients with a mildly reduced heart function, and “there remains reasonable uncertainty about their benefits” in patients with normally functioning hearts.
Atar said an analysis specifically looks at beta-blocker use by patients with a normal heart function will be presented during an American cardiology meeting in November.